Clear Corneal Cataract Surgery and the Correction of Myopia, Hyperopia and Astigmatism
Robert M. Kershner, MD, FACS Copyright.
Eye Laser Center, Suite 303, 1925 West Orange Grove Road, Tucson, Arizona USA 85704-1152, Phone (520) 797-2020, e-mail: kershner@EyeLaserCenter.com
26 Pages
Abstract
Purpose: Advances in cataract removal using topical anesthesia through a clear corneal microincision have created a new opportunity to fully correct refractive errors at the time of cataract surgery. This study was undertaken to assess the effectiveness of keratolenticuloplasty (KLP), the simultaneous modification of the cornea at cataract removal to create emmetropia with lens implantation.
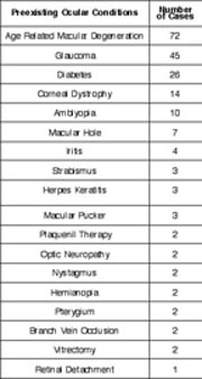
Methods: Data were analyzed for 690 consecutive cataract procedures performed between March 1993 and March 1995 with followup of 12 to 24 months. Each patient underwent cataract removal with topical anesthesia, clear corneal incision fashioned as an arcuate keratotomy to correct preexisting astigmatism, intercapsular phacoemulsification, and microinjection of a single-piece elastic intraocular lens (IOL) into the capsular bag to correct spherical error.
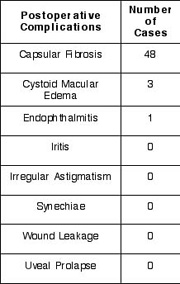
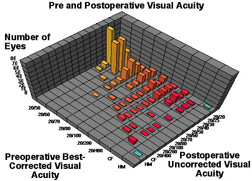
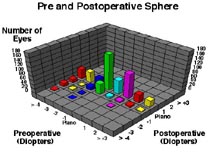
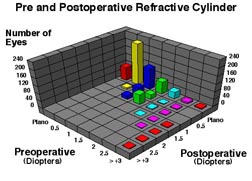
Results: Preoperative, best corrected, visual acuity was less than 20/50 in all patients; 58% were myopic, 32% were hyperopic, and 57% had astigmatism of greater than 1 diopter (D). Postoperatively, spectacle independence was achieved with uncorrected vision of 20/40 or better in 87% of eyes. The sphere was fully corrected in 78%, within 1 D in 17%, and within 2 D in 5%. No patients were overcorrected. The cylinder was fully corrected in 72%, within 1 D in 26% and within 2 D in 2%. Of those with residual astigmatism, there was no significant postoperative shift in cylinder axis. There were no sight threatening complications. All patients were able to resume normal unrestricted activities within twenty-four hours of undergoing the procedure.
Conclusion: The KLP technique can correct spherical and astigmatic refractive errors creating spectacle-free individuals following clear corneal cataract surgery.